Understanding Corneal Dystrophy: A Genetic Eye Condition in Pets
What does it mean when you look into your pet’s eyes and notice something isn’t quite right? It’s natural to feel concerned about your pet’s vision and comfort. One change to watch for could be corneal dystrophy, a hereditary condition that affects the clarity of the cornea. While seeing these changes can be worrying, understanding this diagnosis is the first step toward managing it. This condition often requires consistent monitoring and veterinary guidance to ensure the best possible long-term eye health for your pet.
At Envision More Veterinary Ophthalmology, we specialize in diagnosing and managing complex eye conditions in dogs, cats, and working animals. Our team combines advanced technology with personalized care to deliver precise diagnoses and customized treatment plans. With modern diagnostics and surgical expertise, we’re dedicated to protecting your pet’s vision and comfort through every stage of their life.
Recognizing Cloudy Eyes: When to Suspect Corneal Dystrophy
When pet owners notice changes like haziness, white spots, or a bluish tint in their pet’s eyes, it’s easy to worry about blindness or pain. Fortunately, corneal dystrophy is typically non-inflammatory and often painless in its early stages. Still, timely evaluation is important- other eye diseases can look similar but progress more aggressively or lead to vision loss if untreated.
At Envision More, we use detailed ocular examinations and slit-lamp biomicroscopy to distinguish between hereditary dystrophies and secondary conditions like lipid keratopathy, degenerative scarring, or edema from elevated intraocular pressure. If you notice cloudiness or changes in your pet’s eyes, scheduling an exam ensures accurate diagnosis and peace of mind before complications develop.
What Is Corneal Dystrophy?
Corneal dystrophy is a genetic disorder involving one or more layers of the cornea- the clear, dome-shaped outer surface that refracts light and protects the eye. In affected pets, abnormal deposits of lipids, minerals, or fluid accumulate in corneal tissue, disrupting transparency.
The cornea has three primary layers: the epithelium (outer surface), the stroma (middle collagen-rich layer), and the endothelium (innermost barrier). Corneal dystrophies can develop in any of these, depending on genetic factors and breed predisposition. Although the condition is often bilateral and symmetrical, the degree of opacity and rate of progression vary widely. Some cases remain stable for years, while others gradually reduce corneal clarity and light transmission, leading to vision impairment.
Routine diagnostics and corneal mapping allow our specialists to evaluate the distribution and density of deposits, monitor endothelial function, and customize treatment based on progression and comfort.
How Hereditary Eye Diseases Develop
Corneal dystrophy belongs to a broader group of hereditary eye disease conditions passed through genetic inheritance. It typically follows autosomal recessive or dominant patterns, meaning both parents may carry the defective gene even if they appear clinically normal.
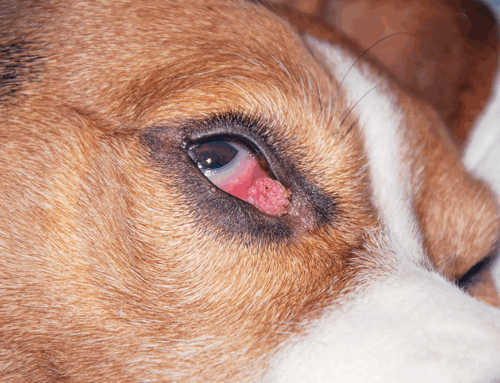
Certain breeds, such as Siberian Huskies, Cocker Spaniels, Boston Terriers, and Beagles, show well-documented predispositions. Canine eye health studies have shown that these dystrophies can appear at predictable life stages- epithelial changes emerging in early adulthood, while endothelial dysfunction typically arises in senior years. Understanding these breed-linked trends allows veterinarians to anticipate risk and begin surveillance before visual compromise occurs.
Our ophthalmology team incorporates pedigree information, genetic testing when available, and long-term photographic comparisons to establish baselines and track progression precisely over time.
Types and Symptoms of Corneal Dystrophy
Corneal dystrophies are classified by which corneal layer is affected and the type of deposit formed. This distinction is critical to determining whether intervention is needed and how to best maintain vision and comfort.
Epithelial and Stromal Corneal Changes
Epithelial dystrophies affect the surface layer of the cornea, often appearing as faint, circular white or gray spots caused by lipid deposition or epithelial irregularity. These cases are generally non-painful and cosmetic but can predispose to recurrent superficial erosions if the epithelial barrier becomes unstable. Chronic cases may benefit from topical lubricants or therapeutic contact lenses to maintain a healthy tear film.
Stromal dystrophies involve deeper collagen fibers and produce a crystalline or “frosted glass” appearance. Over time, these lipid or calcium deposits can reduce transparency and refractive precision, causing glare or hazy vision. Advanced slit-lamp and specular microscopy during ocular examinations help our specialists determine whether deposits are stable or progressive and whether supportive therapy is warranted.
Endothelial Corneal Changes
When the endothelium- the cell layer responsible for pumping fluid out of the cornea- begins to degenerate, the result is corneal endothelial degeneration. This can cause corneal edema, creating a blue-white haze, discomfort, or secondary ulceration as epithelial tissue stretches under fluid pressure.
At Envision More, our ophthalmologists use pachymetry to measure corneal thickness, specular microscopy to assess endothelial density, and optical coherence tomography (OCT) to evaluate microstructural detail. These techniques allow us to detect subtle edema before it becomes clinically apparent, providing opportunities for early intervention.
Diagnosing Corneal Dystrophy
Diagnosis begins with a complete ophthalmic workup. Using slit-lamp biomicroscopy, we examine the cornea layer by layer to determine lesion depth and reflectivity. Fluorescein staining rules out epithelial ulceration, while tonometry measures intraocular pressure to ensure secondary glaucoma is not present.
In certain cases, we may perform corneal cytology or in-vivo confocal microscopy to differentiate between lipid, calcium, and proteinaceous deposits. Accurate distinction between genetic corneal dystrophy, lipid degeneration secondary to hyperlipidemia, or scarring from trauma or infection is vital.
Our diagnostic tools, including ocular ultrasound and tear film testing, support a full understanding of corneal physiology so treatment can be both targeted and minimally invasive.
Treatment and Management Options
There is no definitive cure for hereditary corneal dystrophy, but ongoing management can preserve transparency and comfort for years. The approach depends on disease type, depth, and associated clinical signs.
For mild cases, regular rechecks and lubrication therapy may be sufficient. Artificial tears and hypertonic saline drops can reduce edema by drawing excess fluid from the cornea, while antioxidants or lipid-modifying diets may support corneal metabolism in some patients. When secondary irritation occurs, short courses of anti-inflammatory drops can alleviate discomfort.
Owners can learn how to apply eye drops correctly at home to maintain consistency between appointments. In advanced or vision-threatening cases, surgical interventions like superficial keratectomy, corneal grafting, or endothelial transplantation may restore clarity. Our surgical team specializes in these microsurgical techniques, utilizing viscoelastic stabilization and fine-gauge instrumentation to minimize trauma and optimize postoperative healing.
Differentiating Corneal Dystrophy from Other Eye Conditions
Not every cloudy cornea signals dystrophy. Inflammatory or infectious diseases, metabolic disorders, and systemic lipid imbalances can produce similar lesions. For example, conjunctivitis causes redness and discharge due to inflammation of the conjunctiva, while corneal ulcers are painful, erosive defects requiring immediate antibiotic or surgical intervention.
Corneal degeneration associated with trauma or systemic lipid disorders tends to be unilateral and irregular, unlike the symmetrical presentation of hereditary dystrophy. Differentiation through high-magnification imaging and fluorescein testing prevents unnecessary treatment and helps guide accurate prognoses.
Monitoring Hereditary Eye Conditions Long-Term
Genetic eye conditions like corneal dystrophy require lifelong, periodic monitoring to track subtle corneal changes. Most dystrophies progress slowly, but some can eventually interfere with light transmission or corneal hydration balance. Behavior changes- such as bumping into obstacles, squinting in bright light, or avoiding dark spaces- can suggest worsening opacity or glare sensitivity.
At Envision More, we recommend annual to biannual rechecks for stable cases and more frequent monitoring when corneal edema or ulceration is present. Each visit includes high-resolution photography and corneal thickness mapping for comparison. Early detection of edema, ulceration, or endothelial decompensation allows timely intervention, often preventing surgical escalation.
Because hereditary dystrophies are genetic, we also counsel breeders and pet owners on responsible breeding practices and screening programs to reduce incidence in predisposed breeds.

Protecting Your Pet’s Eye Health
Corneal dystrophy can sound intimidating, but with expert guidance, vigilant monitoring, and appropriate care, most pets live comfortably with little disruption to their vision. Early detection ensures that minor opacities remain stable, and advanced cases can often be managed effectively to preserve quality of life.
At Envision More Veterinary Ophthalmology, we look beyond the immediate diagnosis to safeguard your pet’s long-term comfort and clarity. Whether you’ve just noticed cloudy eyes or are navigating an ongoing condition, our experienced team provides the medical precision and compassionate care your pet deserves.
Contact us or request an appointment today to schedule your pet’s ophthalmic evaluation and take the next step toward clearer, healthier vision.





Leave A Comment